2020 overview
While I was trying to complete the book, I kept getting interrupted by new publications coming out, stimulating new lines of thought. I had to draw a line somewhere, so I chose the end of 2019. Now 2020 is complete, it seems appropriate to look back at what was new during that year. There were four RCTs comparing various types of acupuncture or dry needling with other interventions. I will feature each of them on separate pages in the AcuPHPedia section of the site; here are some general observations.
True to form, we’re keeping up the tradition of heterogeneity. Although all four are RCTs, and two are in the same journal, they have little else in common. Two of them use DN to MTPs but even they use different rationales, different techniques and different muscles!
The conclusions, in short, are:
- Dry needling MTPs in the calf gave added benefit to patients receiving Extracorporeal Shock Wave Therapy (ESWT) [commentary]
- Percutaneous Needle Electrolysis (PNE) gave no added benefit to DN of MTPs [commentary]
- Adding EA to manual needling of Ashi, KI3, BL60 and BL57 gave no added benefit [commentary]
- Electroacupuncture with Warm Needling (EAWN) gave significant benefit compared to waiting list [commentary]
I would like to pick up on the issue of effect sizes.
One of the recent studies (Ho et al) gives us a comparison between the treatment group and a waiting list group. This is the first to have done so, of all publications I have seen on this subject. It gives us some insight into the natural history of the condition, and a baseline against which to compare the outcomes of other studies. Of course, they are not directly comparable, as they come from different populations, in different contexts, yet it is possible to form an impression.
To do so, setting aside the variety of tools and time-frames used, I have focussed on a single measure that they all have in common (morning/first-step pain VAS) and a narrow time frame (baseline to end of treatment/4 weeks). From the data available, I have extracted the group mean scores (ignoring their variance) and calculated the percentage improvement. This is what we get:
(in both charts, the papers are identified by initials, as follows: B = Bagcier & Yilmaz; A = Al-Boloushi et al; W = Wang et al; H = Ho et al.)
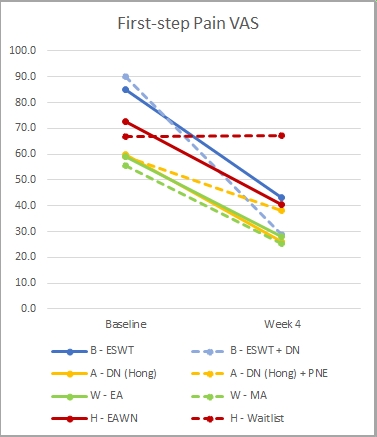
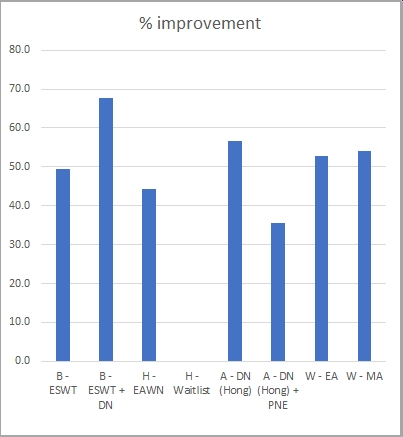
What strikes me here is the overall similarity. All of the interventions, assessed after 4 weeks, were associated with improvements of about the same magnitude (50% improvement +/- 10). This is in clear contrast to the waiting list group that showed no improvement, which seems to suggest that the improvements seen are indeed related to the interventions used. Now we need more studies with waiting list or placebo controls, to back this up.
Please remember this is indicative, not definitive; you need to view the individual papers, to appraise the results properly and to see them in context (e.g. long-term follow-up, etc).
So now let’s look at what new questions have arisen.
1 – Combined strategies. Dry needling to gastro-soleus MTPs gave significant added benefit to an ESWT/cold/stretching/orthosis protocol; how should we build on this?
a – Was the benefit of DN due to facilitating stretching, as intended in this study, or could it have been due to deactivation of MTPs, regardless of stretching?
b – Was the benefit additive, or would DN have achieved the same outcome (or even better) without the ESWT? An earlier study by Eftekhar-Sadat, (needling 2-4 gastro-soleus MTPs, weekly for four weeks) the reduction of pain VAS at 4 weeks was 68.3% – a comparable result, without the use of ESWT.
2 – Interventions at the Ashi point. In the ESWT group the reduction in VAS was about 50%. This is perhaps better than the results of steroid injection (e.g. 45% in Li et al) but seems rather less than the reduction with various other interventions:
- 62% with DN to multiple points in the plantar fascia (Uygur et al, 2018)
- 69% with EA (Kumnerddee and Pattapong, 2012)
- 70% with PNE (Fernandez-Rodriguez et al, 2018)
- 77% with Mini-Scalpel Needling (Li et al, 2014)
This raises the question whether these differences are real, or are due to confounding contextual variables. I guess only direct comparisons will tell us for sure.
3 – EAWN. The paper by Ho et al clearly shows significant benefit of EAWN, compared to waiting list. However, the effect size is small (42%) relative to other studies and this procedure relatively laborious. Also, there are many practitioners who don’t use moxibustion (or are not allowed to, in some hospital contexts). They might ask:
a – what are the relative benefits of different components of this intervention? Is it necessary to include needling, electrostimulation AND warming, or could similar benefits be obtained with less labour-intensive approaches?
b – Are there sub-groups of patients (e.g. with Cold syndromes) for whom moxibustion is particularly indicated?
4 – Practitioner attitudes to invasiveness of interventions. Here is an idea for psycho-sociological research: why do some practitioners (and, indeed, some patients) choose interventions that are inherently painful and invasive, given the existence of benign alternatives? Have they not heard that ‘less is more’?