The multidimensional structure of practice
It has been a while since I wrote here. I’ve been busy focussing on my memoirs and poetry instead. Now I am prompted to post this, to build on a discussion which is being podcasted soon on the Acu-Track site.
First, I want to develop an exploration of the idea of structure which I began in an article that appeared in British Acupuncture Council’s member magazine, Acu1.
I learnt from one of my mentors, Joe Goodman, the osteopathic principle that ‘Structure Governs Function’; meaning that the movement of energy through a system is determined by its structure. Robert Fritz developed similar ideas in relation to mental constructs, in his book ‘The Path of Least Resistance’2, showing how the flow of creativity can be influenced by restructuring how we think. Let’s consider structures relevant to our focus, at some different levels of complexity.
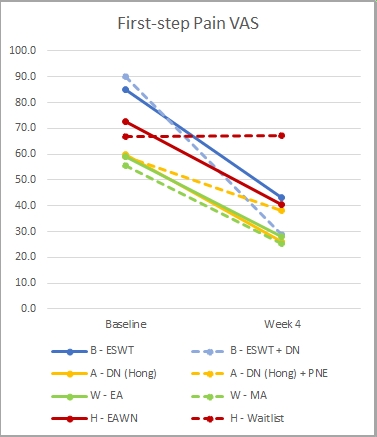
Firstly, an anatomical structure, the plantar fascia of the foot has been blamed for plantar heel pain (PHP). Thought to be due to injured, inflamed, or degenerative, it is taken as the key structural target for interventions such as: injections, shock waves, or acupuncture to the ashi point.
Broadening this slightly, we take adjacent structures into account, and our thoughts flow towards foot orthoses and calf-stretching exercises. Going further, we consider the whole body, considering the tensegrity of the myofascial web, which may lead to needling along the bladder meridian. Other whole-body perspectives include the structure of the nervous system, or the acupuncture meridians.
Looking beyond the individual, we can see structures (or constructs) at higher levels of complexity:
In the clinic:
- Clinic context (availability of equipment, permissibility of moxibustion, etc)
- Consultation (time allotted, frequency of visits)
- The practitioner’s conceptual framework and skill-set
In the lab:
- The inclusion/exclusion criteria for a trial
- Protocols for intervention, and outcome measurement
- Funding channels
And broader society:
- Classificatory frameworks (diagnostic definitions, MeSH terms)
- Regulatory bodies with rules, committees, hierarchy, etc
- Structures constraining what counts as knowledge (NICE, guidelines, protocols for RCTs, systematic reviews, etc).
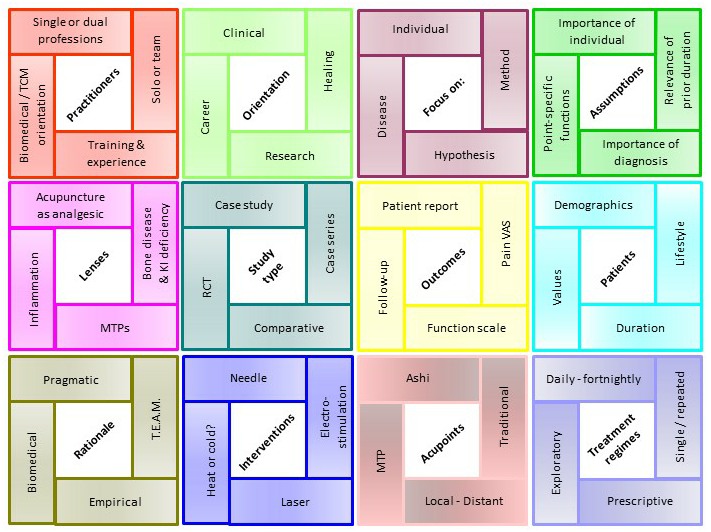
Now let’s put these ideas together with the Patchwork model that emerged from our CIS study3. This model was our attempt to illustrate the range of factors that can influence approaches to the problem (we were looking at PHP, but you could apply this model to other problems too). Within each of 12 areas, four of numerous possible variables are included. You may think this looks too neat – it is. There are other areas that are relevant and other variables that could have been included, and they could all be put together in innumerable ways. The general principle I’m trying to illustrate here is that there is a wealth of diverse factors that can interact in arbitrary ways, depending on context.
Is it useful to apply structural thinking here? I have blogged previously about Anachronistic Categorisations [link], where I critiqued the notion that ‘Calcanodynia is due to bone disease resulting from Kidney Deficiency’. This assumption, or belief, or dogma, is the foundation stone on which a clinical approach is built. If it is found to be incorrect, the whole edifice needs to be abandoned, or demolished, which could be hard, for those invested in its construction.
For another example, let’s consider institutional level structures such as finances, regulations and protocols (another patch that is not in our original diagram but could be added). These impinge on practice in many ways, often unnoticed but shaping what we do. The prevailing culture of evidence-based medicine (EBM) limits the activities of orthodox medics directly, but its influence also percolates down to affect even independent acupuncturists, for example restricting funding by insurance companies to a small range of diagnosed conditions. And the very notion of ‘diagnosed conditions’ pervades the discourse of even traditional acupuncturists.
Further, those diagnostic categories are defined by criteria set by the Powers That Be. There has been a move recently to replace the misleading term plantar fasciitis (PF) by PHP. Some authors started using it, but others have eschewed its use, reverting to the old label because their papers are more likely to be accepted for publication and more likely to show up in literature searches. They do have a point, as we found to our cost; the old jargon is embedded in systems such as the MeSH terms used for searching databases like PubMed. In 2012 we published our systematic review4. This duly appeared in the PubMed database but it was not featured in a subsequent National Institute for Health and Care Excellence (NICE) Clinical Knowledge Summary of the topic. This drew our attention to the fact that someone had failed to include the term ‘plantar fasciitis’ in the MeSH terms, so our paper would fail to show up in any searches limited to that term, and not including PHP. Fortunately, we spotted this and got it changed, but others may not.
I think this illustrates how the structures of the databases (which EBM relies on) perpetuate archaic concepts which, as I showed above, can lead to bad practice. It is as if the various institutional structures – funding bodies, research institutes, publishers, reviewers, databases, etc – are bound together by invisible threads, creating a meta-structure with its own tensegrity, giving it resilience to resist distortion and maintain the status quo.
Now let’s leave this rather analytical way of using the model and consider it more holistically. This image led us to two useful insights. Firstly, a patchwork may be a quilt: a beautiful and useful thing, made of diverse fragments, lovingly and meticulously put together by caring co-workers.
We came across a thought-provoking article by Maura Flannery, describing quilting as a feminist metaphor for scientific inquiry5. She articulated a set of values inherent in a feminist approach, distinct from those of patriarchal science. Viewed from this perspective, it is clear that most of the research on PHP to date is firmly embedded in the patriarchal. The few exceptions are case studies reported by practitioners of Traditional East Asian Medicine (TEAM). I don’t find this surprising, the feminist values identified by Flannery are very congruent with those espoused by traditional acupuncturists, in my experience.
I won’t elaborate on all the values here, as I have done so elsewhere6. Instead I will focus on one, Relationship, because it was this that gave rise to the second insight. What if we gave more attention to relationship, rather than things? Our patchwork image presents the field of research as a number of blocks, suggesting separate fixed entities. What would it look like, as a field of relationships?
Exploring this idea, moving beyond the patchwork structure, I started to imagine a fabric woven from strands of relationship:
- Practitioner to Patient
- Practitioner to Study type
- Practitioner to Orientation
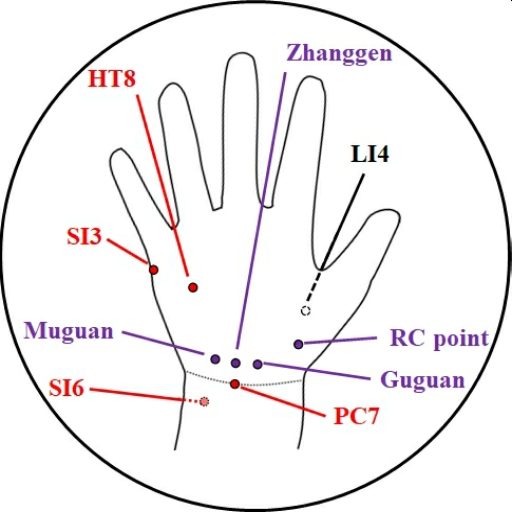
- Practitioner to Acupoints
- Treatment regime to Patient
- Treatment regime to Study type
- Treatment regime to Orientation
- Treatment regime to Acupoints
- Treatment regime to Patient
- Study type to Assumptions made
- Study type to Orientation
- Study type to Acupoints used
- Study type to Patient
And so on,
you get the idea; and there could be relationships with other new ‘patches’ too, such as
- Authors to Publication types
- Funding agencies to Treatment regimes
- Validating bodies to Study type
- Professional organisations to Practitioner orientation
- Lenses used to Symptoms and co-morbidities
- etc
Now here is a thought experiment for you: picture a quilt made of this relational fabric stretched out with a ball rolling on it. If an object is placed on the quilt, it will make a dent, into which the ball will roll. The object represents our initial focus of attention; the movements of the ball show the activities that ensue. The path of the ball depends on where on the quilt the object is placed.
Thus, if you are a person with a painful heel, that will be your focus of attention; your quilt will be distorted accordingly, and person-centred actions are likely to result. By contrast, if you are a policymaker, your starting point will be homogeneity, averages and funding, leading to a very different trajectory. Or, if you are an aspiring researcher, your quilt will first be dented by methodology and criteria for validity.
Let’s take a bit of a leap. You know those images of Einstein’s space-time continuum – grids of lines curved by gravity, wherever there is a significant mass? [see image below] I picture our quilt in a similar way. Instead of a four-dimensional space-time universe, here we have one with many dimensions of interrelationship as illustrated above. Simultaneously, in different parts of this universe, we have distortions centred around each patient, each practitioner, each professional discipline, etc. Like stellar masses they may be light years apart, each constitutes its own solar system which may bear little relationship to the others. Each is a node in our knowledge nexus – each has its own ‘truth’.
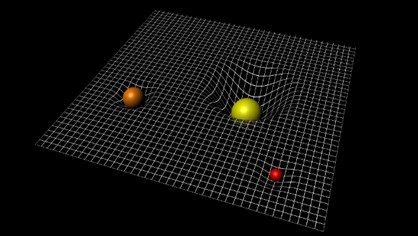
Thus, to Jo Bloggs with their painful heel, the truth of ‘what works’ may be a bespoke approach, based on individual assessment, adjusted week by week as things change, leading to transcendence of the presenting complaint. Meanwhile ‘truth’ for the manager of a cash-strapped NHS clinic may be that a reasonable number of patients will get a good enough outcome if a practitioner with basic training carries out a simple standard procedure. Two truths, very different, as they have emerged from distant galaxies of meaning.
But are truths all equal, or are some more equal than others? In a context where all practitioners are being constrained to stick to a hierarchical evidence base, then this starts to behave like a black hole – making such a big distortion of the quilt that it reaches to every corner, all galaxies of meaning are forced into orbit around it.
So, what is to be done? Should we all jump in our spacecraft and hightail it to the rebel bases at the periphery of the Universe, out of reach of the black hole? Or can we instead use this model to raise awareness of how the structures we inhabit constrain our reality?
I honestly don’t know where this goes next. Is the quilt merely a metaphor, or can we make it a useful model? Does it make sense to you? What are your ideas about the issues it raises?
I would love to get your input on this and hope to see you in the forum.
References
- Clark R. Structural influences on practice, viewed from the heel. Acu 2021; 32: 24-25. Opinion.
- Fritz R. The Path of Least Resistance: Learning to Become the Creative Force in Your Own Life. Fawcett; Rev ed. edition (1 April 1989), 1989.
- Clark MT, Clark RJ, Toohey S, et al. Rationales and treatment approaches underpinning the use of acupuncture and related techniques for plantar heel pain: a critical interpretive synthesis. Acupunct Med 2017; 35: 9-16. DOI: 10.1136/acupmed-2015-011042. Full text
- Clark R and Tighe M. The effectiveness of acupuncture for plantar heel pain: a systematic review. Acupunct Med 2012; 30: 298-306. DOI: 10.1136/acupmed-2012-010183. Full text
- Flannery MC. Quilting: A Feminist Metaphor for Scientific Inquiry. Qual Inq 2001; 7: 628-645. DOI: 10.1177/107780040100700507.
- Clark RJ. Advances in acupuncture for heel pain: towards integrative practice and research. Birmingham, UK: Independent, 2020.